3Q with Lydia Bourouiba: How has our knowledge of the coronavirus changed since last spring
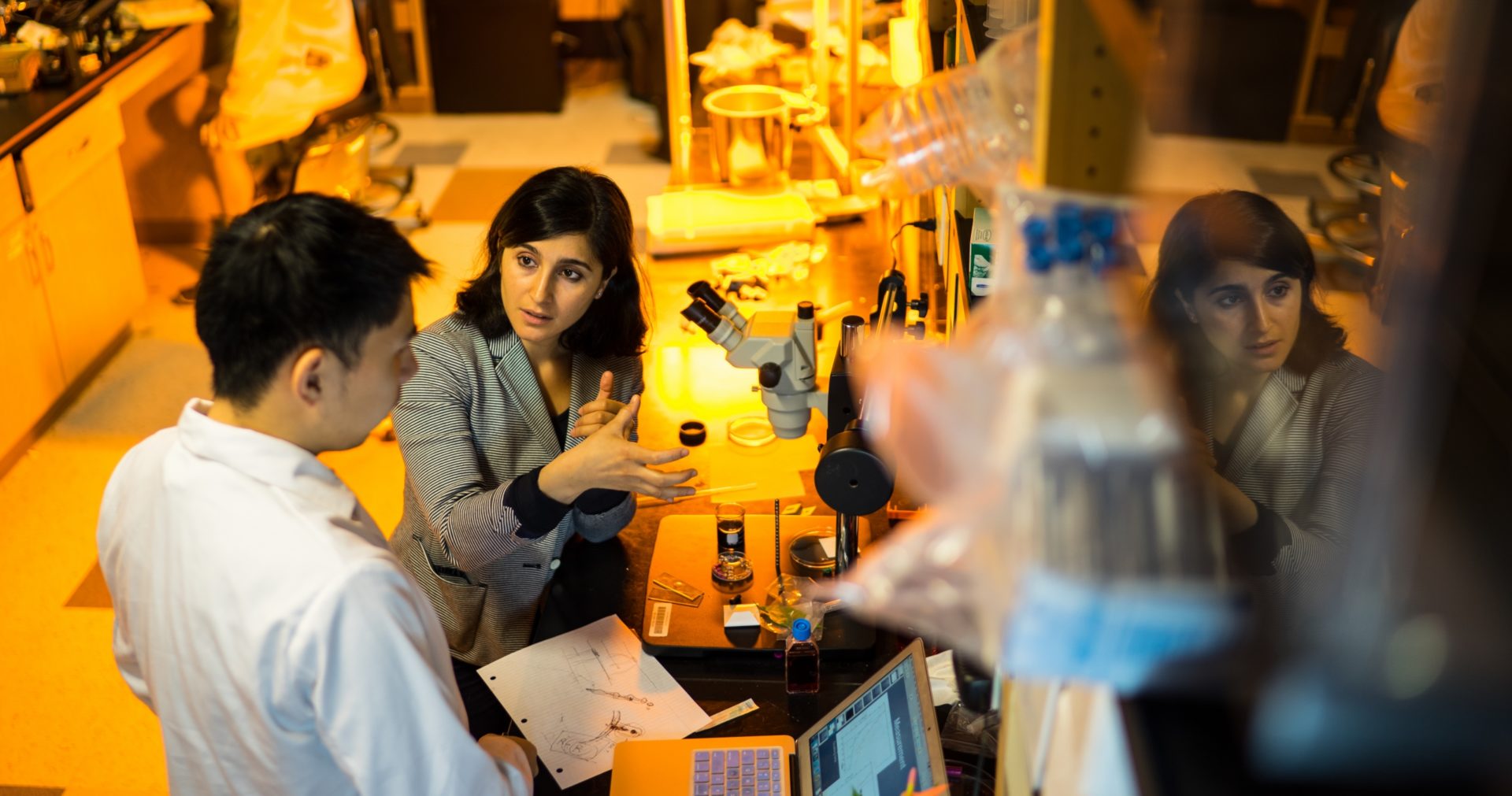
Lydia Bourouiba is an Associate Professor in the Department of Civil and Environmental Engineering at MIT, where she directs The Fluid Dynamics of Disease Transmission Laboratory. Her research and contributions in 2020 led to a newer understanding of respiratory emission dynamics and had implications for mask and respiratory design, social distancing recommendations, and other public health interventions during and after the COVID-19 pandemic. Professor Bourouiba sat down to share insights gained from her research over the past year.
Q. How has our knowledge of the virus changed since last spring and what has that meant for your work?
A. Many things changed, and some didn’t. Most of the changes we have seen in terms of our knowledge are, in part, related to the pathology and the reaction of the immune system — how the virus interacts with the body is one of the keys for patient treatment. Another aspect is the ability to develop vaccines currently being deployed. Compared to historical precedent, this was done in a very short timescale of one year. Even with the massive effort it took to do that, we’re not really going to see the level of deployment that we would want to see for probably another year. The last important piece we have learned relates to knowledge about transmission; we now know that SARS-CoV-2 is definitely not just transmitted via large drops over short distances as was originally claimed. There is a very important component of transmission that occurs through inhalation of what remains in the air after a cough or sneeze and there are a number of questions remaining about that and the environmental conditions that promote or inhibit such routes of transmission and how much certain locations or indoor spaces enhance such routes of transmission versus others. We know that the airborne route definitely contributes significantly to transmission, but we still need more information to understand precisely how and what biophysical mechanisms are at play. So, we learned a lot but there is a lot that we still need to learn if we are serious about improving future prevention and mitigation of the spread of this pathogen.
Q. People are now being vaccinated but it will be some time before society is safe enough to return to normal. With the winter months still ahead, how can people avoid spreading coronavirus in indoor spaces with poor ventilation?
A. We still have a long road ahead of us before the vaccine covers the percentage of the population that we need in order to prevent further spread and stop the pandemic. In the meantime, indoor spaces that are poorly ventilated are a major issue and improving those situations should be of the highest priority. This could require making full infrastructure upgrades if the means are sufficient to do so, but if not, there are low-cost ways to improve natural ventilation and localized filtration systems that are more affordable. Steps should also be taken to minimize the number of individuals that occupy such indoor spaces, making sure that those who are vulnerable are not in contact with others that are highly and actively connected and interacting with many others regularly. So, essentially applying high standards of control and mitigation with respect to occupancy, face covering, air and surface hygiene, and distancing remain critical. Wearing high-grade masks is also an option for individuals that are at particularly high risk. Finally, it will be important to enable full and sufficiently homogeneous air changes in rooms with poor ventilation by opening the windows and ensuring adequate patterns of air circulation at regular intervals, even in the winter.
Q. Is there anything we can learn from this experience to avoid future outbreaks causing such global problems?
A. First, we shouldn’t repeat the pattern of past epidemics or pandemics in which within a year a resolution of the COVID-19 crisis we would see a return to completely ignoring the issue of infectious diseases and risks of epidemics and pandemics of respiratory infectious diseases in particular. We must ensure that there is more investment in monitoring and prevention in addition to massive efforts in developing vaccines. We need to think more holistically. It’s not just about vaccine development because as you can see, even with a historic level of resources, coordination, and some of the biggest pharmaceutical companies of the world coming together, we still need at least two years in the best-case scenario before an emerging pathogen that causes a serious pandemic can be tackled with a vaccine. In one sense, we were lucky with SARS-CoV-2 because another virus could have transmitted just as easily but with a much higher death rate. We are currently experiencing a bad-case scenario, but it’s not the worst-case scenario and we know that these pathogens will keep emerging. We need a strong mobilization system for early detection information-sharing worldwide so that the very early cases for such new emerging pathogens are identified and information is centralized and can be used quickly. But we also need a chain connected to that, ensuring proper investment in prevention before we even know what the pathogen can really do and to ensure that a system is in place to minimize the risk of worst-case scenarios triggered by high-frequency transmission settings that we know can occur. That’s something that I think we really need to think about from a societal standpoint, and which would have a big impact in terms of not having entire areas of the economy shut down before a vaccine is deployed, if it becomes available. Such holistic investments in early detection and prevention of transmission would have a big return on investment because the economy would simply be much more resilient, even when facing new pathogen threats.
One other piece that is really important to touch on is the need for fundamental research; often it is not obvious early on what will become important when a crisis hits. It is thus critical to fund research that sometimes does not necessarily look ready for immediate application. The type of research I do and have started years prior to this pandemic was not particularly popular in terms of funding but ultimately a lot of the insights we gained were helpful in guiding key policies and implementing mitigation strategies. So, the importance of investment in fundamental science and early vision, even when it’s not immediately applicable is critical to also keep in mind because when we face new challenges, it is often the insights from such research become or drive part of the solutions.
Share on Bluesky